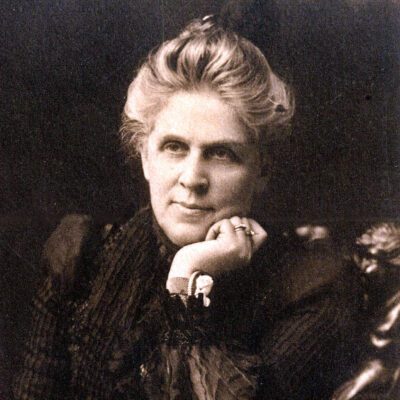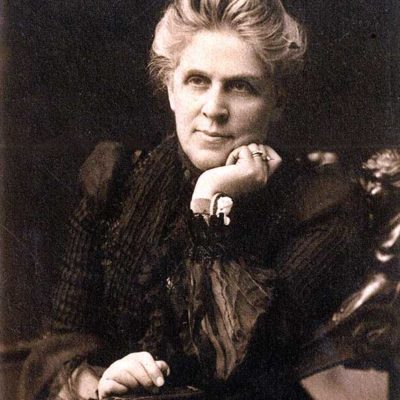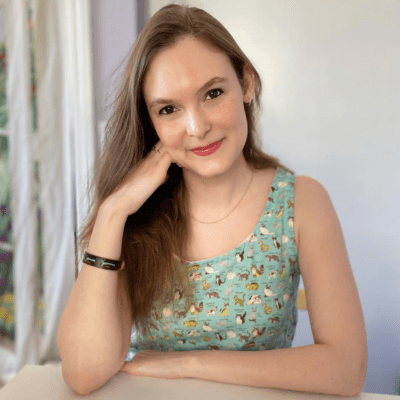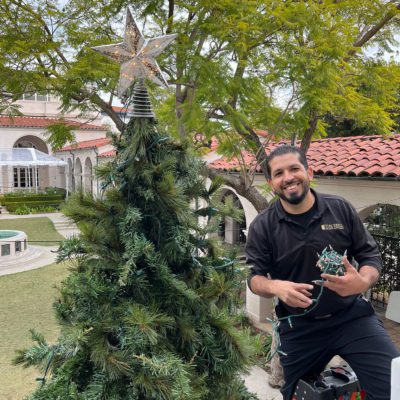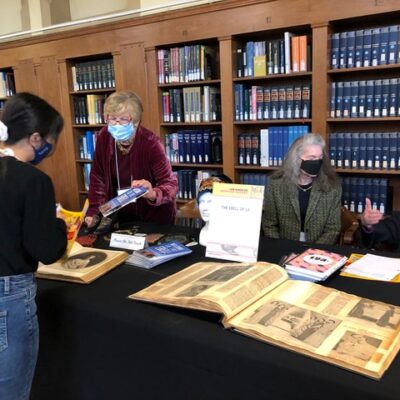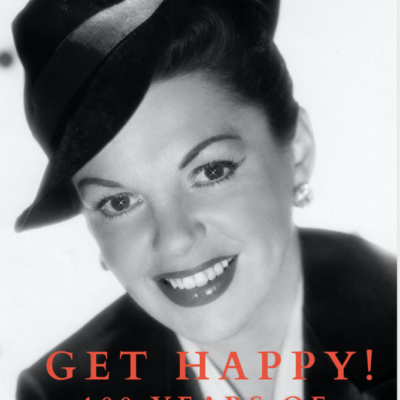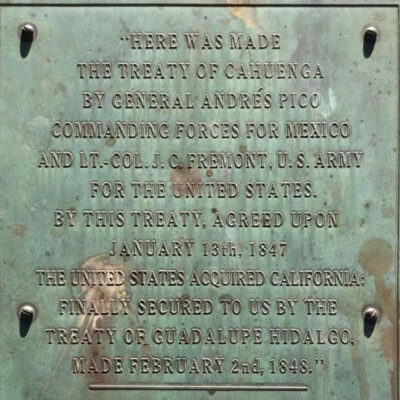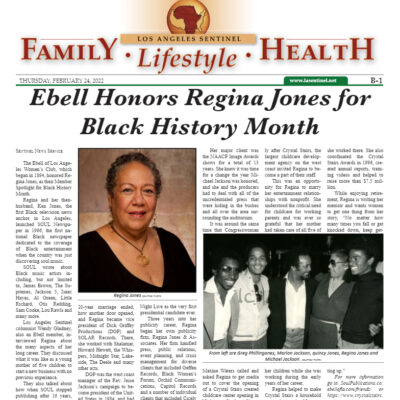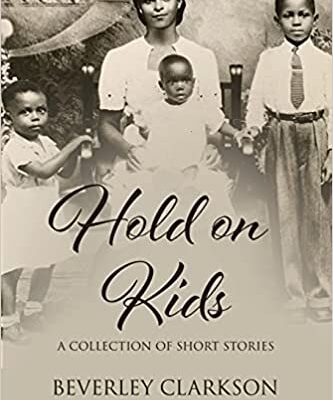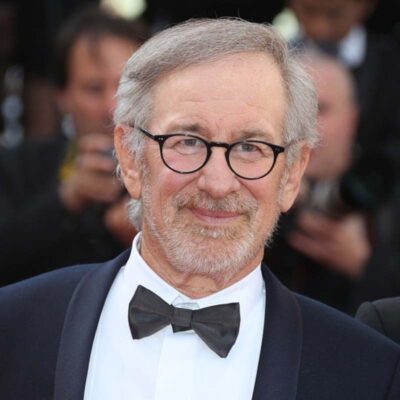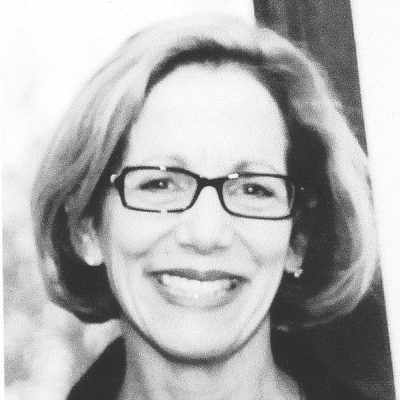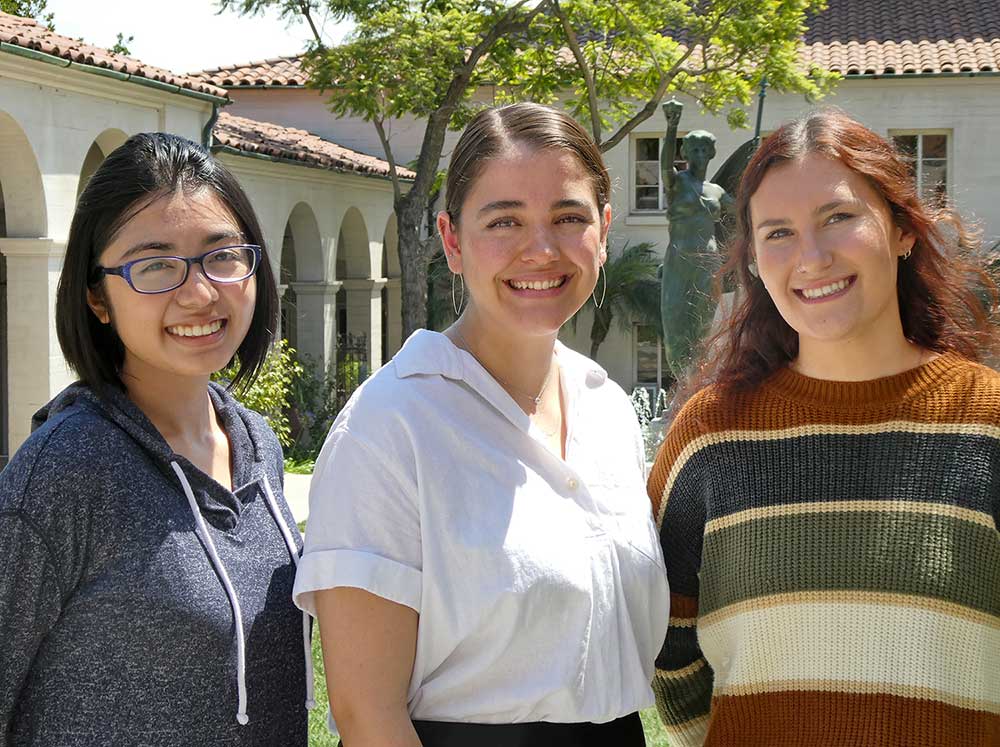
(left to right) Jasmine Gonzales, Angelica Seifert, Abigail Knight
An Interview with Three Ebell Scholars
In this time of the COVID pandemic, much attention has been paid to the far-reaching repercussions it has had on the medical community. We’ve all seen stories in the press about burnout and medical staff, especially nurses, leaving the profession due to the tremendous strain of caring for COVID patients. Currently the Ebell has eight scholars working on a degree in nursing, seven of whom are attending Mount Saint Mary’s University (MSMU). We wondered how nursing students are coping with their studies and what insights they may have about their chosen profession. We invited three of our nursing scholars to sit down with us at the Ebell for a conversation about their experiences and their views of where they feel the profession is headed as we slowly emerge from the pandemic.
We discovered three exceptional and articulate women who have a passion for their profession. All three are in MSMU’s 4-year Traditional Bachelor of Science in Nursing program. Abigail Knight (Abby) and Angelica Seifert (Angelica) were accepted as Ebell Scholars with the class of 2020/21. They are currently seniors and will be graduating in the spring of 2023. Jasmine Gonzales (Jasmine) was accepted as an Ebell Scholar with the class of 2021/22 and is currently a junior and will be graduating in the spring of 2024.
In addition to their clinical work, Angelica and Abby work at UCLA Medical Center as Care Partners, which is similar to a CNA position but non-certified. This provides them more opportunities to learn and apply their nursing skills and knowledge. From the beginning of her journey to becoming a nurse, Abby excelled. She was accepted into the California Nursing Students’ Association, which provided her with a mentor and other support that has helped her excel in her nursing studies. Jasmine was valedictorian of her high school graduating class. She has completed her first year of clinical work at UCLA/Ronald Reagan and at Providence St. John’s Hospital. Despite having the responsibilities of helping raise her two younger siblings, Angelica graduated summa cum laude from College of the Canyons High School with AA degrees in Mathematics and in Liberal Arts & Sciences with a Social & Behavioral Sciences emphasis.
What areas of nursing are you planning to pursue?
Angelica plans to become a pediatrics nurse and went into nursing wanting to work with kids. Abby initially considered pediatrics. She has a younger sister with serious health issues whom she has helped take care of, and has always loved working with kids. But she loves the ER, the fast pace and the challenges. “It’s exciting and you feel good when you have a good outcome, and you still get to work with kids.” In order to become an ER nurse, she would first start out in medical surgery, then the ICU. Jasmine isn’t entirely decided yet, but is interested in pediatric nursing. Abby commented, “If you start out in OB or pediatrics, you can’t easily change. To go from treating kids to adults is like starting your career over again.”
How has the pandemic affected your academic program and your experience doing your clinicals?
One effect has been the struggle to get clinical assignments. Nursing schools are scrambling to get clinicals assigned and faculty are scrambling to find the needed placements for their students. As a result of staffing changes and shortages, hospital administration wants smaller groups of nursing students. This has led to an increase in online instruction and a decrease of in-person instruction. Another change is the schedule. In many of the hospitals where nursing students complete their clinicals, the standard 6-to-8-hour weekday shift has been replaced with a 12-hour weekend shift. “This creates schedule conflicts with our job hours. And if you miss a shift because you contract COVID, they’re not very understanding,” Abby commented. During the COVID shutdown, 50% of clinical hours could be done online, but now 75% has to be onsite to qualify for required hours.
Jasmine feels her clinical experience this past school year wasn’t as hands-on because the nurses are too busy due to understaffing to provide the level of supervision clinicals normally afford. Abby and Angelica concurred that staff at both UCLA Medical Center where they work and at the hospitals where they’re doing their clinicals are out because of sickness, retiring early, or leaving the profession. Some of Jasmine’s peers had to move to get clinical experiences, while others were not notified of placement until the last minute. Many hospitals where they used to go, now don’t want students because of being short staffed. Still, she feels she’s able to provide comfort care to patients and free up nurses. She shared one example of an elderly patient with dementia with whom she was able to form a bond because she was the person the patient saw most often. “Patients are directly affected by short staffing.”
All three agreed the clinical training current nursing students receive is less than what pre-COVID students received. Abby expressed her concern of not having enough opportunity to practice necessary skills (e.g., hanging an IV drip, administering certain meds) because nurses just don’t have sufficient time to teach that. Even with all the difficulties they’re experiencing, at the end of a shift they are getting thanks and appreciation from the nurses for their help.
Has the pandemic as a potentially ongoing public health condition shaped your long-term nursing goals?
Jasmine feels the COVID pandemic has deepened her commitment to her chosen profession because taking care of people is a large part of her identity, growing out of her family role of caregiver to her younger siblings. “I have this passion to care for people. I’ve seen how nursing has helped my family. I’m the eldest and I’ve used my nursing knowledge to care for members of my extended family. Nursing is a fulfilling job.” Angelica does not see herself in another role. “It’s in my blood. Nursing is a very independent career that requires a lot of critical thinking and working on your own,” she added. All three admitted some days end with them crying for what they’ve experienced. Angelica recently learned a patient she’d worked on had died. Naturally, she felt very sad, but also gratified she was able to help the patient. Abby also recently experienced the loss of a patient, and is not sure she could take the heartbreak of losing a child patient on a regular basis. But no matter how hard, at the end of each shift they come away with a feeling of contributing good to the world and a sense of confidence that they can make a difference.
What are your opinions about people who choose not to vaccinate and/or follow COVID protocols? And what do you feel is needed to better prepare us for the next public health crisis?
Abby expressed her view that people often defend such choices by saying it’s their individual decision, but framing it in that way shows their unwillingness to acknowledge the dangerous effect it can — and often does — have on the larger community. “I wish they would come to work with me and see the type of people who are being hospitalized and intubated. They are the unvaccinated.” She cited her own sister, who’s unable to be vaccinated for health reasons, as an example of who may be negatively affected by others’ “individual decision.” Angelica sees this issue as a lack of respect for public health and for health care workers, as well as a lack of trust in health authorities such as the Centers for Disease Control, which traditionally people explicitly trusted. “It feels like a slap in the face sometimes when people say I’m not going to get vaccinated.“ She stressed that such people don’t understand the risk nurses, or anyone in the hospital, put themselves in from those who are not vaccinated and come to the hospital. “If we’re going to be better prepared next time, we need much more education about the importance of public health. People need to be educated on how our public health system works and maybe that would build a stronger sense of trust in public officials.”
Abby and Jasmine agreed that better education could help dispel some of the misinformation. Jasmine expressed her dismay of people within the medical community who remain unvaccinated and spread misinformation about the vaccines. “I find it really upsetting because these are the people who should be educating others.” She cited the importance of teaching best practices, such as checking multiple, credible sources before making such high-risk choices about one’s health. Abby agreed adding, “Social media has promoted a lot of education and provided a lot of good information. I learn new stuff everyday. It is true some people use social media to promote false information, but people need to learn how to discern what’s good information.”
You’ve all chosen nursing, a traditional field for women to enter, as your profession. What is this generation of women bringing to the profession that earlier generations perhaps didn’t?
Angelica cited one of the biggest differences as the “expectation of equality” that nurses have. “We won’t take less than. I am fighting for more than. We don’t expect sexism and we’re willing to fight for what we need. In the workplace, I’m not going to present myself as a woman; I’m going to present myself as a professional individual.” As a female-dominated profession, Abby acknowledged the troubling history of nurses being sexually harassed on the job by doctors, co-workers, patients and how that is absolutely not tolerated now as evidence of this expectation. “This generation of nurses will immediately report to authorities; they’re not afraid to speak up and report because you cannot treat me as less than professional.”
Angelica also noted there’s “a lot more two-way communication between doctors and nurses, and nurse-driven protocols are more common now because nurses are taking more of a leadership role in patient care.” She added that nurses have more agency when it comes to advocating for their patients and for themselves. Jasmine agreed, saying she feels this generation of nurses “has more confidence to speak their mind and will not tolerate any disrespect.” Until she began her clinicals, she didn’t realize how little doctor/patient interaction there is compared with nurse/patient interaction. “Doctors only see patients briefly, and often nurses present to the doctor what is going on. Patients trust nurses and are more open to telling nurses what’s going on with them.”
If these three dedicated young women are representative of the future of nursing, then the profession is clearly in very capable hands. The Ebell should feel proud that we have been able to play a small part in helping to secure that future with our scholarship.